Final Infusion & Economics of Cancer Treatment
The second and third phase of treatment, which started in April 2022, has been a bit of a journey. But after 62(!) total infusions, I completed my final immunotherapy infusion on Wednesday, 3 December 2025. I feel good about finishing the treatment course, and I hope that this was the last time I have to sit an in infusion bay. To mark the completion of the infusions, I got to rang a bell and received a certificate. It was nice to have a number of the oncology nurses gather around and cheer me.
Note: I think “Loong” is in quotation marks because that is my preferred name in their database. I’m not sure if they realized that “Loong” is my middle name, rather than some odd derivation of “Weng”.
Emotions & Mentality
While I am happy and relieved, finishing the maintenance immunotherapy infusions does not feel as significant as when I finished either radiation course (IMRT in 2018 and SBRT in 2023) nor the chemotherapy courses. I think the reasons for not feeling more accomplished are two-fold: i) I’ve been fortunate to be quite tolerant of the immunotherapy, and ii) not much will change following the completion.
The main side effects for me have been fairly minimal - some itchy skin rashes that can be relieved with a topical cream. In contrast, the first radiation course took a big toll on me and Aiday. In 2018, when there was broader radiation to my mouth and neck, I lost 40 lbs because eating was so painful and slow. I had so little energy back then - both during the radiation and subsequently with the chemo. From April to August 2022, when I went through systemic treatment, the effects were also rough, since that treatment included chemotherapy. I had to take drugs to combat the nausea and there were days (granted, predictable) when I had low energy. The completion of SBRT in 2023 also felt more significant in that that treatment was trying to kill a cancerous tumor. For that treatment, I had to lie completely still for 45 minutes because such concentrated doses of radiation were targeting the tumor. In contrast, the maintenance immunotherapy part of treatment did not result in any significant health challenges. I felt relatively good throughout the immunotherapy - I could drive myself to appointments, exercise, travel and do normal activities before and after. The main annoyance was the 4-6+ hours every 6 weeks to commute to UCM, wait for the bloodwork results and pharmacy clearance, receive the infusion (only 40 minutes in total) and commute back home. Healthwise, there were no expected changes in my bloodwork or scans as a result of the treatment.
Going forward, not much will change now that I’ve finished my last infusion, as there are no side effects that will improve. I will still have to continue to take levothyroxine for the rest of my life to treat hypothyroidism. Dr. Rosenberg, my medical oncologist at UCM, said the damage to the thyroid is essentially permanent. My daily pill is supplementing ~50% production. I’ll continue to have to have regular blood tests to potentially adjust the dosage, based on any changes.
The other reason why the last infusion does not feel as significant is that I could have stopped sooner if I wanted. Most patients on immunotherapy are only on the treatment for two years. I’ve been taking pembrolizumab for 3.5 years - the first 6 months were part of systemic treatment, then a year of maintenance when the tumor was mostly gone, then two years of maintenance after the SBRT. I had a natural ending point in August 2025, but I decided to continue to the end of the year, as insurance had already approved and I wanted to do everything possible to make sure cancer does not return.
As in 2018, I have to make a bit of a mental transition. There is a sense of reassurance in going to the hospital and seeing doctors and nurses on a regular (every 6 week) basis. Having my blood tested regularly and having nurses and doctors to answer questions about my symptoms and how I was feeling was helpful. I am still scheduled to have follow up appointments every 3 months, though that is not as frequent as every 6 weeks for infusions.
After the clear scan in December 2018 and the doctors told me I was “cancer-free”, I thought of myself as no longer a cancer patient. At that time, I thought of myself as someone who’d battled cancer and won. This time, though, even as I’m no longer in active treatment and have had a series of clear scans, I still think of myself as a cancer patient, albeit one not actively receiving treatment. At this point, I feel that there’ll always be a risk that it may come back, so I’m quite reluctant to consider myself “cured.”
Even if I don’t consider this a “major” milestone, it is nonetheless a reason to celebrate. Aiday, Charles and I went to Moody Tongue, in no small part due to them serving one of our favorite desserts - the 12 Layer German Chocolate Cake. Charles, not for the first time, attacks this cake as soon as it arrives on the table. There is no need for utensils in his mind.
Economics of Cancer Care
Following up on post about Keytruda stick shock (17 June 2022), I reviewed my medical claims and the payments around my infusions. The 62 total number of infusions I’ve received breaks down as follows:
Treatment (2018): 5 chemo infusions of cisplatin and carboplatin. This was used in conjunction with the radiation - weekly basis
Adjuvant (2018): 6 chemo infusions of carboplatin and 5-FU to help prevent cancer from returning post-radiation - 2 drugs on monthly basis
Systemic treatment (2022): 23 chemo and immunotherapy infusions total to treat the recurrence of cancer. The drugs were carboplatin, gemcitabine and pembrolizumab - 6 cycles of 3 weeks each (with infusions on day 1 and day 8 of the cycle)
Maintenance immunotherapy (2022-2025): 28 pembrolizumab infusions every 6 weeks from August 2022 to December 2025
If you’ve ever been curious why cancer centers seem so nice (especially relative to other departments within a hospital) or why there are new cancer centers being built, the discussion below may help to explain it. In summary, cancer patients are a hospital’s cash cow, so cancer centers will compete for patients. Of course, having state-of-the-art facilities, cutting edge research, ancillary services, and social support networks will benefit the patients and their families. But the cancer centers and hospitals who serve them benefit financially, to a great degree.
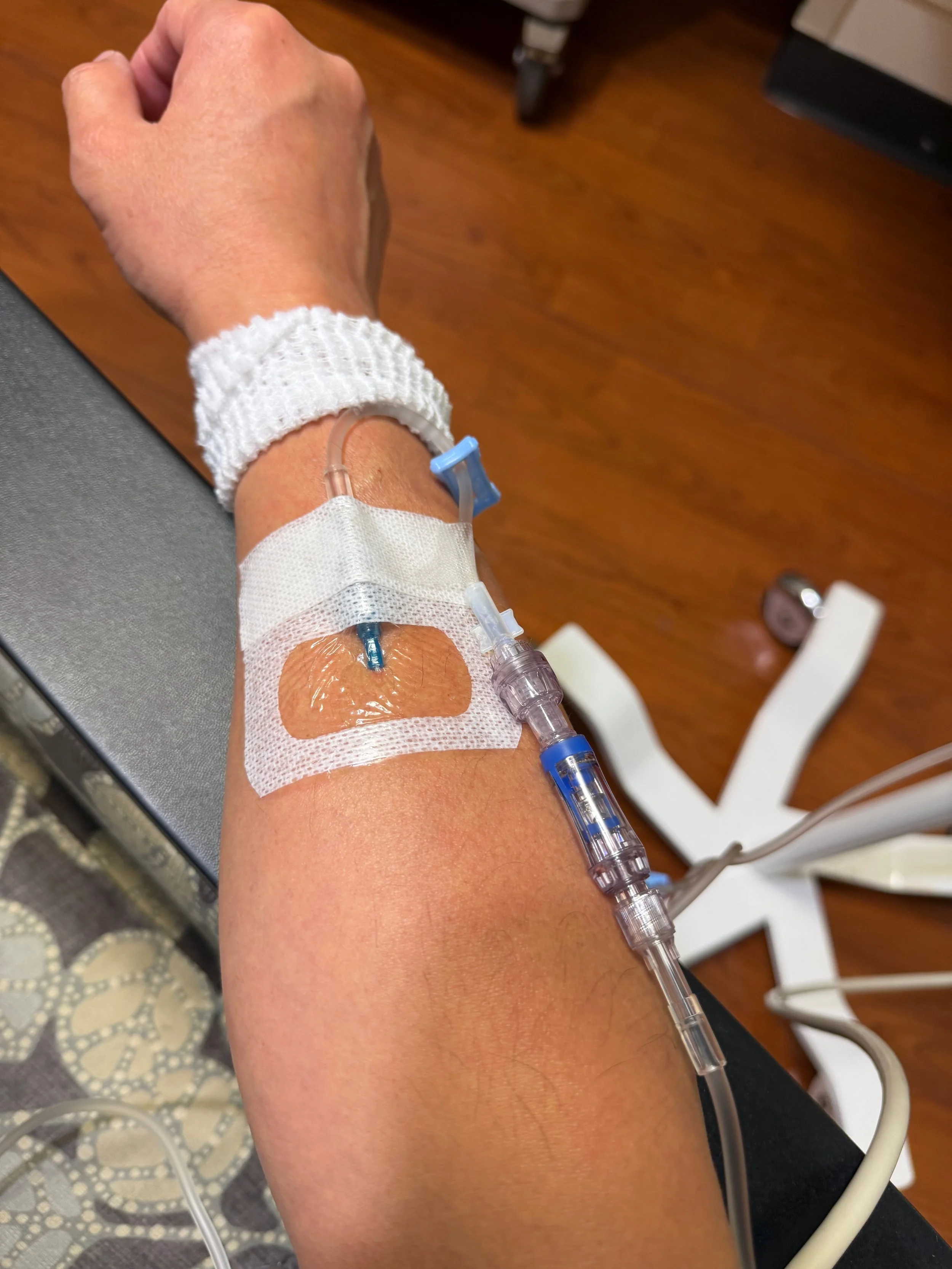
As an infusion patient, since 2022 University of Chicago Medicine received payments from insurance for over $1.5 million dollars related to my infusions alone. For my maintenance IO, I was worth $400,000 per year to UCM - $50,000+ for each of my 8-9 infusions per year. In addition, they received payment for the blood tests needed to clear me for treatment and the consults with the oncologist, PA and nurses during those visits. My visits were relatively straightforward and didn’t require any sophisticated procedures or particularly advanced skills. A specialty nurse had to find a vein in my arm and properly insert an IV to deliver the drugs. The drugs were then delivered through the IV while I sat in the room by myself.
Another aspect I found a little odd was how the payment doubled when I went from the 200mg dose every 3 weeks to the 400mg every 6 weeks. For the 200mg dose, UCM would bill out around $80k and get reimbursed ~$26k by insurance. For the 400mg dose, UCM would bill out at around $160k and get reimbursed $54k by insurance. The administration of the drug is no different but somehow insurance agrees to pay double. It was just more convenient for me not to have to go as often. I still remained baffled by why insurance (in our case Aetna) is willing to reimburse at a rate more than double Keytruda’s list price of $24,000 per dose given every 6 weeks.
To put this into context, the insurance paid MD Anderson a total of $73,000 for my SBRT treatment in August 2023, including the treatment planning, creation of the radiation stent and custom masks, and the 4 doses of targeted radiation. The treatment program requires highly sophisticated planning to precisely shape and deliver the correct doses from different machines to the tumor while minimizing damage to the surrounding tissue. In addition, the maintenance of the linear accelerators and lasers is necessary for them to work as accurately is required. During the each radiation session, there was a team of 4 technicians, in addition to Dr. Phan and his team, who were monitoring the treatment in real-time. While the radiation does was only a few minutes, the total time in the machine was closer to 45-60 minutes, as I had to precisely positioned and scanned before each dose. So I can understand why a SBRT treatment could cost on the spectrum of healthcare services - the training of the doctors and technicians carrying out this treatment as well as the cost of the radiation machines is high. Certainly much higher than an infusion pump.
SBRT machine is much more advanced than an infusion bay
Even if $73,000 for SBRT may been seen as a relative value compared to $50,000 immunotherapy, I can’t help but think about the costs in Singapore. The quoted cost for SBRT treatment at the National Cancer Center was around $22,000, a fraction of the cost at MD Anderson. That’s also only half the cost of a single immunotherapy infusion! And I’m sure the cost of immunotherapy infusions is a fraction of what it costs in the US.
Well, this is a relatively short update post, as we’ve reached a milestone. I’m still working on the other updates, so hope those will be posted shortly. Thank you again for reading and for your support.