Two Year Scans
It’s been a bit too long since my last update in May. Since then, I’ve made two trips to MD Anderson in Houston (August and November) and have had other appointments locally. I will break up the updates to three separate posts: a) update with respect to oncology and scans; b) update on long-term side effects and dysphagia; and c) food highlights.
Overall Highlights
August 2025 marked the two year post-SBRT treatment milestone. The good news is that that the scans remain clear, and there are no signs of tumor progression or recurrence. This is certainly the news we are hoping for and comes as a relief. That being said, neither scan appointments was as straightforward as we would have liked.
In terms of the long-term side effects, the swallowing issues have become a bigger concern. Specifically, not all food and liquid is not going straight down my esophagus - some is escaping through my nose and some is getting stuck. Because of the radiation, my palate does not form a tight seal with my throat. The next post will detail the efforts to address this, including filler injections and a prosthetic device called an obturator. In the first few days of usage so far, the obturator has been beneficial.
The third post in this series will be around the Texas travel. In August, Aiday, Charles and I decided to make a short vacation out of it, so we went for 8 days, including a short trip to Austin. Yes, Texas in August is as hot as it sounds! We ate a lot of great BBQ that trip. For the November trip, I went solo to Houston for 5 days. Both trips featured a lot of great eating, so that post should hopefully be mouth-watering and have more pictures.
Scans and Medical Oncology
August 2025 - Dr. Gillison
Note: This section will be chronological, as I had written some of this earlier this summer.
As usual, my appointment schedule at MD Anderson in August was very efficient - all done in a single day. The day started with an MRI at 6am, and then I had appointments with speech pathology, ENT, radiation oncology and medical oncology. I was done by around 4pm, so even earlier than usual.
In summary, the scans remained clear, with no signs of recurrence or progression. At this point, the news is more of a relief than a feeling of elation. We got the news from Dr. Maniakas, my ENT, at around 11am, so the rest of the day was getting confirmation from the oncologists. My appointments tend to be pretty straightfoward at this point. There isn’t any discussion about treatment plans or expected changes, and the goal is just to maintain the status quo.
Along those lines, my appointment with Dr. Phan was relatively quick. As the scans are clear, there was nothing to show me from the MRI (whereas previously he could show me side by side images of the tumor and various stages). With me being 2 years out from the SBRT treatment, Dr. Phan only needs to see me every 6 months, as he does not expect any changes. His prognosis for me is quite encouraging.
My happiness with the good news of clear scans was tempered by the news around Dr. Gillison, my medical oncologist. On my appointment schedule, I had noticed that I was scheduled to see Jennifer Owens, Dr. Gillison’s PA. I had assumed that Dr. Gillison was going to be on vacation or at a conference. However, we found out that Dr. Gillison took a leave in July. She had informed MDACC in August (the week of my visit) that she was not going to return to see patients. Jennifer could not disclose any more information, but she said to send our thoughts to Dr. Gillison. Without knowing any more, this sounds serious and not merely a case of her moving institutions.
Dr. Gillison has been our most trusted doctor throughout this phase of treatment. I really like and appreciate her expertise and her manner. As a world class and pioneering researcher (she is one of ~10 faculty at MDACC who is a member of the National Academy of Medicine), she speaks from a position of authority. She has the credentials and confidence to make very clear recommendations, such as when she told us in no uncertain terms that the treatment plan offered by UCM was unnecessary. During our appointments, she always responded thoughtfully and thoroughly to my questions. She did it in a way that I could understand and that was medically precise - she didn’t dumb things down for me. I liked having to look up certain terms to figure out exactly what she was saying. She was both realistic and encouraging. We relied on her opinion to guide the course of treatment and manage our expectations.
Previously, we had discussed how long to remain on immunotherapy. Dr. Gillison discussed how there aren’t really any studies of patients who’ve been on immunotherapy for longer than 2 years. Based on the current studies, the benefits of immunotherapy are durable and long-lasting. In other words, the body’s immune system is trained well enough to act, even if the patient is no longer actively receiving the drugs. In addition, drug companies don’t want to approve longer-term / indefinite treatment, so there isn’t a sizable patient population that has taken IO for longer than two years.
I may be a bit of unique case in that I started immunotherapy in April 2022, as part of my systemic treatment with chemo. So I’ve been on IO for 3.5 years already. We had discussed finishing the treatments after my September 2025 infusion (two years post-SBRT). However, without Dr. Gillison’s direct advice and with my insurance having already approved infusions through the end of 2025, I figured to do the additional treatments. My reasoning is that a) I tolerate the drugs well, i.e. limited side effects beyond occasional mildly irritating skin rashes and b) I don’t want to have any second thoughts about not doing everything I can do ensure the cancer does not return. Going back to 2018, I was initially disappointed that I was not randomized into the control group - the group that did not get additional adjuvant chemotherapy post-radiation. Instead, I was assigned to the group that had to receive 3 more rounds of a rather tough chemo drug (5-FU), which was administered through a pump I had to wear and carry around with me. This followed a pretty tough 7 weeks of radiation, during which I lost 40 lbs and had trouble eating. While I didn’t enjoy it at the time, if I had not done that additional chemo, I would have always wondered if the cancer came back because I didn’t do enough. Using that same logic, I want to make sure I do as much as I can now to reduce / eliminate that sense of questioning.
With the plan to eventually come off immunotherapy, the medical oncology team at MDACC wants to monitor me every 3 months (vs. seeing Dr. Phan and radiation oncology every 6 months). Thus, the schedule to return in November 2025 vs. February 2026.
November 2025 - Elevated Anxiety
This trip was initially scheduled as my typical Tue/Wed (11-12 Nov) visit, but without radiation oncology on the schedule. However, the visits were extended to Mon-Fri (10-14 Nov) since I wanted to see oral oncology to have them fabricate the obturator (more on this in an upcoming post).
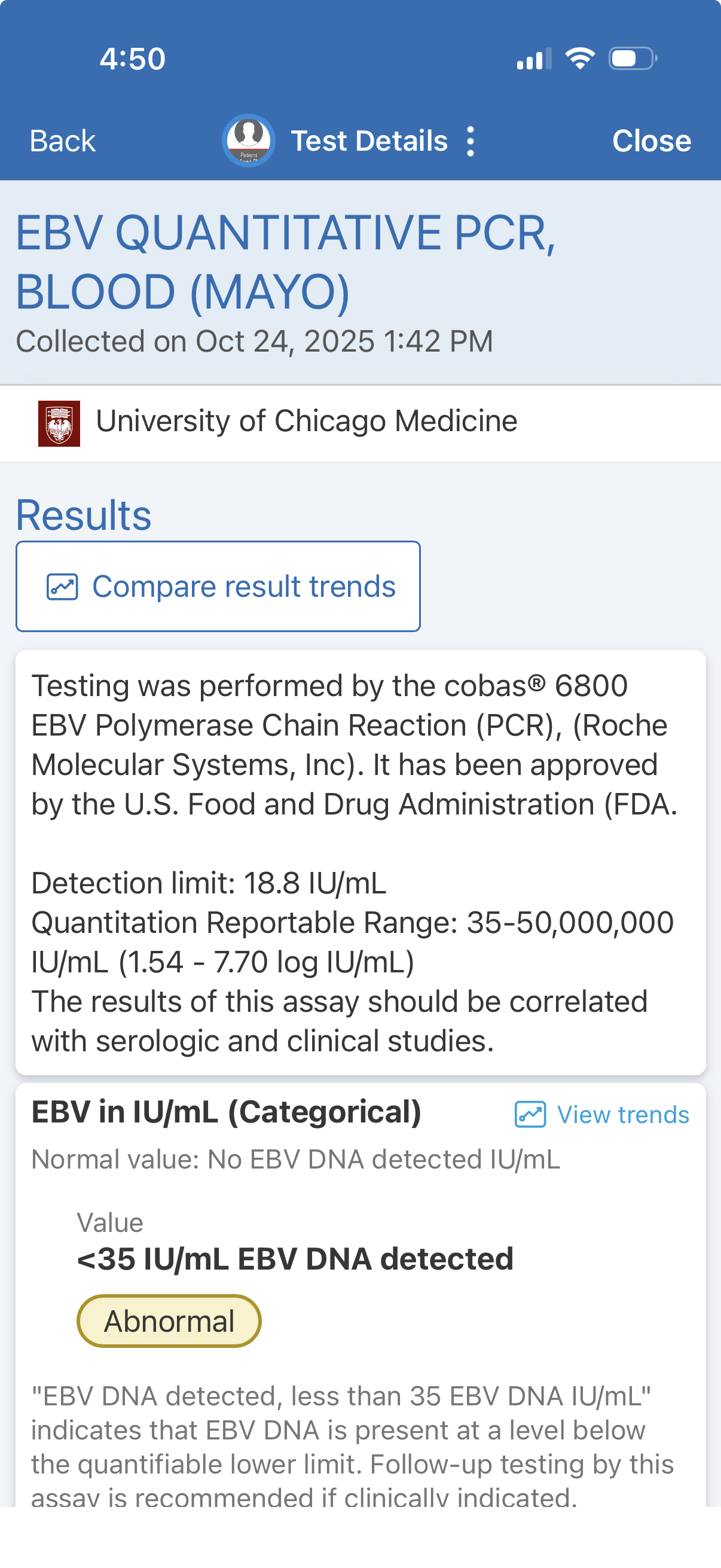
Subsequent to the August visit, I had infusions at UCM on 10 September and 24 October. As part of my bloodwork, I get an EBV test. As a reminder, my tumor was EBV positive, so the blood tests are a way to potentially identify the return of the cancer. The results of my 10 September test were negative - “Not Detected”. However, the test on 24 October returned an abnormal result - EBV was detected, though below the quantifiable threshold. I had become so accustomed to the “Not Detected” result that I didn’t even check the test result until 6 November. So in a way, I was blissfully unaware for several days and could enjoy Halloween and other activities without the additional anxiety.
This result was the cause of elevated anxiety for a few days
I was also fortunate in that I was scheduled for scans at MDACC on 12 November, so I “only” had a week of elevated stress. While Dr. Phan and the oncologists did not expect the tumor to return, I still had concerns after seeing the EBV test results. After all, the cancer wasn’t supposed to return after my 2018 treatment. Even though there were plausible explanations - general fall sickness season, I had gotten vaccines for flu, Covid and shingles between my infusions - those did not totally allay my concerns. Mentally, I did not go to the darkest places, though I was concerned and probably more irritable during those days. The effect of the test result was to make me hyper-sensitive to everything going on in my right ear. I spent the weekend wondering whether the little pressure changes / perturbations in my right ear were the result of a tumor. I probably would have dismissed those concerns as normal if not for the positive EBV result.
To further add to my stress, traveling from Chicago to Houston on Monday, 10 November was not the smoothest. Instead of a relaxed afternoon flight, I was scheduled for a 5:10am flight, as I had a Monday afternoon appointment. In addition the FAA flight reductions (nominally due to the government shutdown), Chicago got ~6in of snow overnight. When I woke up at 3am, I saw that my flight was cancelled, and I had been rebooked on a flight that was scheduled to arrive around 9pm that night - meaning I would miss my Mon appt. I went to Southwest’s app and managed to book myself on a 5:55am flight to Austin, with a connection to Houston arriving at 1:10pm. I still might be able to make my 2pm appt. As I suspected the 5:10am flight was one of the casualties of the FAA flight reductions, I figured I would go to Midway and try to catch the 8am direct MDW-HOU flight. As it turned out, about 85% flights that morning from MDW were canceled, likely due to the snow, and the next direct flight to Houston was in the evening. I was really lucky to get on one of the flights that actually left.
Only 11 of 76 scheduled flights departed from Midway on Monday morning (at 4:31am)
After landing in Austin around 8:15am, I decided to change my car rental and drive to Houston, about 3 hours away. I would definitely make my 2pm appointment (with time for a nice lunch, to boot), and I didn’t want to hang out in the Austin airport for 4 hours. Also, MDACC’s travel agreements allowed me to pick up in Austin and return in Houston without any extra charges, so that was a bonus.
The oncology part of my visit started on Wednesday, 12 November. I was supposed to start at 8am with labs but when I sat down and asked what they were drawing, the EBV assay was not in the orders. In hindsight, I should have messaged the team in advance so that they could add it. Instead, I spent a few hours calling and waiting for the test to be ordered. I was hoping that the EBV test would come back “Not Detected” sometime on Wednesday so that I could relax a little more before seeing the oncologist on Thursday. However, I didn’t get my blood drawn until ~1:30pm, and I did not get results that day, so that prolonged my uncertainty a little bit longer.
On Thursday, I finally met with the oncologist. As I suspected, my blood pressure was elevated - as high as 170/110 on the first reading. I did come down a little a few minutes later, but certainly not to the 120/80 zone.
To add to the anxiety, I was taken to the exam room a little after my 9:30am appointment time. I waited, and waited, and waited - I wasn’t seen until after 11am. Because of the positive EBV test, I started to wonder whether I wasn’t being seen because the conversation would be longer than a routine, clear scan. That’s the impact of the abnormal EBV test.
I met with Dr. Laura Chow, an oncologist whom I had not seen previously. Going into the consult, I had more nervous energy than previous appointments with oncology. Fortunately, the radiology reported “stable post treatment changes…without suspicious enhancement.” What a relief after all the anxiety!
The latest EBV test results were unknown during the appointment, so Dr. Chow ordered a precautionary PET scan for February, in case the test showed elevated levels and I became symptomatic. A few days later, the EBV test came back - “Not Detected”. The clear MRI scan and that resulted eliminated the remaining concerns about recurrence, so I’ll plan to cancel that scan.
The one outstanding question is who will be my medical oncologist at MD Anderson. Dr. Chow told me that she is merely covering for doctors on maternity and paternity leave. So I’ll have to check back with MDACC to see who will be my regular doctor going forward. Logistically, a doctor who has clinic the same days as Dr. Phan would be preferred, so that I can maintain the efficient schedule.
In summary, the scans remain clear and my prognosis remains optimistic. I am planning on doing my final immunotherapy infusion on 3 December 2025. In some ways, I’ll miss the reassurance of getting regular blood tests and seeing the doctors and nurses at University of Chicago. It’ll also be nice to think that at that time, I will no longer be an “active” cancer patient receiving treatment but will instead be moving towards a monitoring phase.
Thank you again for reading. I’ll plan to have the next two updates in the next few weeks. Hope you have a happy Thanksgiving.