Upward Trends
Overall, the results of my latest regular follow up scans and consultations at MD Anderson from 22-23 April 2025 continues to be good, with clear scans and an optimistic outlook. The scans remained clear and did not show any signs of recurrence or progression. Further, there were no indications of perineural spread (growth along a nerve). Both Dr. Phan and Dr. Gillison believe that there is a high likelihood that I’ll remain cancer-free through my next scheduled scan in August, which will mark the two-year anniversary of the SBRT treatment. That is an important milestone (assuming no tumor progression or recurrence) for two reasons: first, the chance of recurrence is lower after that point, as Dr. Phan said that 90% of cancers that come back do so within the first two years of treatment; and second, the treatment plan would be to stop immunotherapy at that time. So I am in the “home stretch” in the words of Dr. Gillison.
Once again, it is quite a relief to hear that the scans are clear. Even though that is sort of the expectation now - I do not detect any changes in energy or pain that would be an indication of a tumor - it is reassuring to confirm that with the scans. As I’ve mentioned previously, I enjoy talking with Dr. Phan and Dr. Gillison, as their experience and expertise give me confidence that I’m doing about as well as can be expected for a patient with my history.
Health Challenges - January and February
Immediately after my last post in January, I had a few health challenges. Namely, I had i) flu & pneumonia, which required another hospital stay, ii) a brain MRI and iii) setbacks in my jaw / swallowing capabilities.
During my regular immunotherapy on 25 January, I felt fatigued and feverish. The next morning, I had no energy at all and I was burning up - my temperature was 103F! Per my post surgery recovery instructions, we went to Northwestern’s ER, as my fever was well over 100F. After a few hours wait (city center ERs are quite depressing places, even at 10am on a Saturday), I was admitted and spent the next 3 days (2 nights) in the hospital. Thus, during an 11 day stretch (17-27 Jan) starting with my surgery in Houston, I spent 5 days in a hospital (and getting to eat hospital food!).
I was diagnosed with flu and pneumonia. I believe the post-surgery protocol was to make sure my body wasn’t reacting to a surgery-related infection, but this seemed coincidental with a bad flu season in Chicago. At NM, I spent the first night in sort of a temporary holding area on the mezzanine floor. It was not the best room, I had to use a bathroom down the hall, and I could literally see all the foot traffic outside the window. The second night, because I am a cancer patient and had just received an infusion the day before, I got transferred to the oncology floor. This was on the top floor of Prentice, with my own private bathroom and much nicer views of the city. The doctors actually wanted me to stay for a 3rd night. That would not normally be a bad idea, as I could more easily isolate from Aiday and Charles. However, they both were diagnosed with the flu over the weekend as well, so we all had it. Thanks to in-part my tamiflu shot, I was further along in my recovery than them, so I took my discharge on Monday night.
In early February, I had a visit with a UCM neurologist, as this as scheduled as the “urgent referral” related to my intractable hiccups. When I saw Dr. Graf, we barely talked about the hiccups, and she administered a series of neurological tests. One of them was to stick out my tongue. She noticed a deviation to the right. While I thought it was almost certainly related to the effects of radiation, she wanted to be sure that it wasn’t anything more, so she ordered an MRI of my brain, out of an abundance of caution.
As a veteran of MRIs (not necessarily a good thing, like being called a “veteran of the NBA draft lottery”), I was fine to do another one. (Unlike CT scans, MRIs do not use radiation, so I wasn’t getting any more of that.) However, during this MRI, I had spasms in my jaw muscles. They didn't cause big movements, but I was concerned that they would affect the images. Fortunately, the tech said the scans were fine. Apparently the MRI Brain did not reveal anything concerning, as I did not need a follow up visit with the doctor who ordered it.
The jaw muscle spasms are an example of other setbacks I’ve had with respect to my swallowing and speech functions. As my recovery from the thyroglossal duct cyst removal surgery required no neck strain, I had to pause much of my rehab exercises for ~2 weeks. That is when I started noticing greater frequency of swallowing issues and my jaw muscle weakness. In terms of swallowing, I notice that I now cough up more food that isn’t fully swallowed. In particular, fruit like apples and oranges are harder to swallow now. For the jaw muscle weakness, for example, when I am engaged in prolonged conversation, my muscles start to fatigue, and I need to pause for a few minutes to allow them to relax. Otherwise, my speech becomes slurred and less intelligible than usual.
Houston Visit - April
I think of consultations in two categories: 1) oncology and 2) quality of life and side effects management. For oncology, the appointments include the MRI, bloodwork (EBV test) and visits with Dr. Phan and Dr. Gillison. For the quality of life and side effects management, those visits are primarily with speech therapy and ENT - Dr. Maniakas and his team.
In terms of oncology, the “home stretch” is starting to come into view. The follow up plan has moved from every 3 months to every 4 months, with my next visit planned for August. After that, I’ll be on a 6 month interval for the next 2 years and then annual starting in year 5. As mentioned, the treatment plan is to continue on immunotherapy until August. After that, Dr. Phan plans to have me on a vitamin E and pentoxifylline drug regimen. This is intended to help reduce the longer-term side effects of the radiation treatment.
My first appointment following the MRI scan was with Dr. Maniakas and his team. He first wanted to follow up on the TDC surgery. Very good news on that front, as the scar is healing nicely and their muscles around my neck remain soft. As he planned, the scar is along one of the natural skin folds in my neck, it doesn’t stand out much. I do really like Dr. Maniakas’s manner and care. A few weeks after surgery, he called me in the evening to check in, respond to some questions I sent via MyChart and provide some additional care instructions.
Scar from thyroglossal duct cyst is healing well
While oncology remains quite positive in the outlook, I do have quality of life issues that I am actively addressing. I am experiencing more of the long-term side effects of radiation, mostly from the 2018 course (as a reminder, that was 70 Gr of total radiation administered to my head and neck over 7 weeks). These side effects are expected, but as Dr. Gillison noted, there aren’t long-term studies to provide a guideline for what I should expect. There are two reasons for this: a) there isn’t funding to study patients >5 years post-treatment and b) the patient population with my background (particularly two courses of radiation - more than 100 Gr total) is small. Dr. Gillison said that immunotherapy is extending the life of many patients, so there are more people like me and I am “not a red headed Eskimo.” So while there are case studies, there isn’t a study to an answer to my question of what does the trajectory look like for the progression of side effects.
For me, the main side effects of the radiation include the following:
dry mouth (xerostomia)
nasal regurgitation
swallowing issues
tongue vesticulations and weakness
muscle stiffness / fatigue, particularly on the right side of my jaw
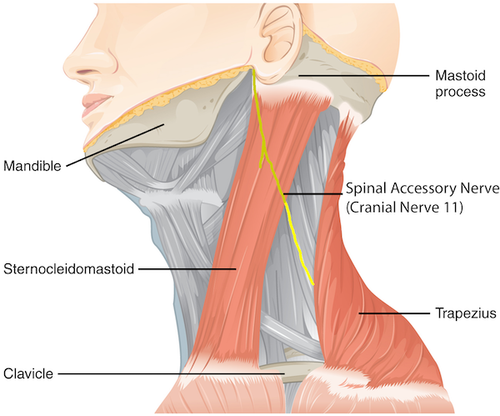
right shoulder weakness, particularly the trapezius muscle, and scapular winging
The good news is that the MDACC SLP I met with this time - Esther Volmer - said that my neck still remains quite soft and that I don’t have lymphedema, though I do have fibrosis. This was in concurrence with Dr. Phan’s examination. I had re-engaged with my physical therapist at Rush a few weeks ago, and we’ve been working on a number of exercises to stretch and build strength in my neck and shoulders. The team at MDACC want me to continue that program.
Until this visit, I didn’t realize that the jaw muscle tightness and the right shoulder/trapezius weakness are both related to the same underlying issue - damage to my spinal accessory nerve (SAN) from the 2018 radiation. I had thought that the shoulder weakness was more related the frozen shoulder I had a few years ago. However, the doctors explained to me that the SAN innervates both the sternocleidomastoid and the trapezius muscle. So two major muscles impacted by that one nerve!
While we had brief prior discussions about getting botox injections to help relieve the muscle spasm issues, at this point, the plan is to try to manage the jaw stiffness with manual therapy (massage) and stretches. Unlike the nasal regurgitation, this issue it still more in the nuisance / mild annoyance category, and it doesn’t affect my day to day functionality. If the condition worsens, then we can re-assess.
As all the doctors, SLPs and PTs say, my goal is just to try to maintain my functionality as much and for as long as possible. I’m hoping that there is a plateau and I’ll stay on it for a while. But there aren’t any assurances that the side effect progression doesn’t continue linearly or becomes significantly worse at some point. I’ll just have to re-double my efforts on the rehab program.
As far as rehab, the TonguePress is one exercise that needs renewed focus. During my visit, my max tongue pressure dropped from 48-50 in prior tests (back in Dec) to 40-42 currently. In addition, when I press my tongue to the inside of my cheek, there is asymmetry - there is greater pressure on my right cheek and less on the left. This is all consistent with have greater radiation on the right side of my neck and face. There is some concern that I have radiation damage to the CN XII nerve that innervates my tongue.
Spinal accessory nerve
The issues that affect me most on a day-to-day basis are the dry mouth and the nasal regurgitation. I’ve tried most all of the products for dry mouth, with the xylitol lozenges being my preferred relief currently. While dry mouth is not as much of an issue when I’m home, it does present more of a challenge when I’m traveling. I do try to have water or liquids with me at all times, but when I don’t, the effects of dry mouth aren’t pretty. It results on a build up on my teeth and lips - there is no saliva to help clear them. I have to remind myself to wipe those clean before taking pictures. The expectation was that I’d lose 20-50% of my salivary glands after the 2018 radiation. Initially, I thought/hoped that I’d lost only 20%, but now I think I’m at the upper end of that loss range.
Dr. Phan’s team provided a few things to try. First, they re-iterated the benefits of the baking soda rinse. The rinse is alkaline, so that may be beneficial in stimulating saliva production as well. Second, they recommended acupuncture as a treatment. This seems to be supported (or at least not contra-indicated) by studies, so I’ll have to start that again. Finally, they gave me samples of another OTC product called Smart Mouth, so I’ll try that as well and see if it might be helpful.
The other major issue is nasal regurgitation (I think the medical term for this is velopharyngeal dysfunction, or “VPD”). Even before discussing the eating issues, Dr. Maniakas said that my voice sounded more nasally than last time, indicating that air was escaping through my nose. As my nasopharynx does not close properly, food and drink ends up going up into my nose and not down my throat. This issue is starting to rise above a “nuisance” levels of discomfort to being more problematic. It is happening more frequently. For fluids, especially when I drink while I still have food in my mouth, the fluid can come straight out of my nose. This is not a huge issue when I’m drinking water - it just looks like I have a watery, runny nose. But when I’m drinking tea or red wine, it does look weird - and has a chance of staining my clothes, if I don’t catch it in time. For food, nasal regurgitation is an irritant. Small foods like rice, noodles, spices, broccoli florets, for example, end up in my in my nose, which makes me want to sneeze or blow my nose. Both the dry mouth and the nasal regurgitation means that it takes me longer to eat than normal, as I it takes longer to swallow certain foods and I have to manage food that doesn’t always go down smoothly.
I went to my SLP at Rush prior to my visit to MDACC. He did an endoscopy with colored water to assess and video the issue. In addition, he confirmed what the MDACC team also suspected - that my soft palate moves well and symmetrically. The problem for me is that the back of my nasopharynx is a little stiff and does not close as it should.
Fortunately, there is a treatment to address this. Dr. Kobayashi, a fellow working with Dr. Maniakas, provided the details of this. The treatment would be to inject a filler to bulk up the area to increase the likelihood of that area closing and preventing food and fluid from coming back up. He suggested doing a first treatment with a shorter duration filler - one lasting 6 weeks to 3 months - to ensure that it provides the expected benefits. Then I would get longer lasting fillers - 3-6 months - to address this issue. This is an outpatient procedure with local numbing anesthesia, so the most significant side effect is pain. The downside, though, is that this is another chronic condition that may require lifelong management, analogous to having to take a pill for my hypothyroidism and needing ear tubes for the eustachian tube drainage issues.
This is a procedure I have yet to do. On the one hand, I trust the team at MDACC to do the procedure. On the other hand, this sounds like something that needs to be done 1-3x / year, so I’d prefer to have someone in Chicago with expertise to do this. The team at MDACC said that while this procedure is not novel, it is also not common. They suggested trying to find someone with a laryngology fellowship (like Dr. Kobayashi, though he is moving on from MDACC in June). I’m hoping to find someone with this type of relevant experience in Chicago.
The filler injection procedure and adherence to the exercise program will have the most impact on quality of life over the next few months. I still need to find a good routine for the maintenance rehab program, as I have different exercises for tongue, swallow, jaw mobility, and shoulder stability & strength.
Medical Industry
I had an interesting conversation with Dr. Gillison about various aspects of the medical industry. In terms of research funding, she said that NCI studies are typically funded to study a) acute toxicities for 180 days, b) quality of life for 2 years and c) survival rates for 5 years. In this political environment, she said that MDACC is feeling the effects of the funding cuts. Since the overhead costs are now capped at 15%, MDACC is losing ~$100M in research funding from that change alone. She is also concerned with cuts to post-doctoral training funding, there is a risk to losing the half of the next generation of doctors, especially if these cuts do beyond the next 4 years. She wonders where those doctors will go, since pharmaceutical companies are also cutting their funding in response to the policy changes. Sort of stating the obvious, she didn’t think that people were voting for cutting cancer research and killing people.
Quick Notes on Eating & Travel
While the first few weeks after returning from Houston were tougher than usual, I recovered fully. Further, we’ve had some great trips to Mexico City (4 days of food indulgence) and Japan (2 weeks in Tokyo and Kyoto - my first time outside the airport). Both were amazing trips. I’ll have to write more about this later.
For this short trip to Houston, I stayed with our friends in Friendswood, which is near the NASA complex. It worked out well that I was able to try a place nearby called Viola & Agnes Neo Soul Cafe. This is a Creole restaurant (one of my favorite types of food - I even did a solo eating trip to New Orleans a few years ago) that was named in NYT Restaurant List of 2024 (50 places across the US). The gumbo was really excellent - spicy and depth of flavor - topped with a crab claw, a chicken drumstick and a hard boiled egg. The fried catfish was cooked expertly and the sticky chicken special were also tasty. I wish my stomach could have handled more, like the etouffe. The place has more of a dive bar feel to it and didn’t have much in the way of desserts, so no bananas foster for me.
On Wednesday, because my visits to MDACC were so efficient and on-time, I finished in early afternoon. I had an MRI, blood draw, and 4 consultations between 7:15am and 2:15pm, so I was able to both move up my flight and visit another restaurant. Conchinita & Co is a casual Mexican restaurant on the way to the airport, so I had a margarita and their namesake conchinita pibil dish. It was a nice way to celebrate the good news from the visits.
Thank you again for reading this and for the support. I am feeling good - no pain and no energy change - and without symptoms and hopefully this continues. The radiation side effects are manageable, though it requires more visits to rehab and an extensive home program, and I’m able to enjoy traveling, eating and most thing as before. We have fun plans for the summer and I’ll keep you updated.